When your little one is miserable—fussy, congested, or breaking out in a rash—it’s easy to jump to the conclusion that allergies are to blame. But figuring out what's truly an allergic reaction in a baby can be tough. So many of the signs look just like a common cold or other typical infant troubles.
The real giveaway is the pattern. You're looking for symptoms that just don't quit, like a runny nose that never seems to dry up, skin irritation that lingers, or consistent tummy trouble right after they eat.
Decoding Your Baby's Allergy Symptoms

Think of your baby’s brand-new immune system as an overzealous security guard in training. It’s still learning to tell the difference between a real threat (like a virus) and a harmless visitor (like pollen or a protein in milk). An allergic reaction is just that system mistakenly flagging a harmless substance as a dangerous intruder and launching a full-blown defense.
Learning to read these signals is the first, most crucial step toward getting your baby some relief. A cold will usually run its course in a week or so, often with a fever. Allergy symptoms, on the other hand, can stick around for weeks or even months without one.
To help you connect the dots, here’s a quick checklist of common signs organized by how they might show up in your baby.
Common Infant Allergy Symptoms Checklist
| Symptom Category | Signs to Watch For | Common Triggers |
|---|---|---|
| Skin Reactions | Dry, red, itchy patches (eczema); raised, itchy welts (hives); sudden puffiness around eyes/lips. | Foods (milk, soy, eggs), environmental factors (pet dander, dust mites), lotions/soaps. |
| Respiratory Issues | Constant runny/stuffy nose with clear mucus; frequent sneezing; itchy, watery eyes; a dry, persistent cough. | Pollen, mold, dust mites, pet dander, secondhand smoke. |
| Digestive Distress | Vomiting, excessive spit-up, diarrhea, mucus in stool, extreme gassiness or colic after feeds. | Cow's milk protein, soy, eggs, wheat, peanuts, tree nuts (often via breast milk). |
This table is a starting point, but let's dive a little deeper into what these symptoms actually look like.
Skin Reactions to Watch For
A baby’s skin is incredibly sensitive, so it's often the first place an allergic reaction makes itself known.
- Eczema (Atopic Dermatitis): Look for patches of skin that are dry, red, and intensely itchy. In babies, this often appears on the cheeks and scalp first, then might spread to the crooks of their elbows and knees.
- Hives (Urticaria): These are unmistakable raised, red welts that can pop up suddenly anywhere on the body. They look a lot like mosquito bites and can come and go quickly.
- Swelling (Angioedema): This is a more concerning sign. You might notice sudden puffiness around your baby’s eyes, on their lips, or even on their hands and feet. This warrants a call to your pediatrician.
Respiratory and Nasal Clues
It’s completely normal for parents to worry about respiratory symptoms, but it's important to know what you’re looking for.
One of the biggest clues that you're dealing with allergies and not an illness is the absence of a fever. If your baby has a temperature, you’re almost certainly looking at an infection. But if you have those cold-like symptoms for weeks on end with no fever, allergies are a prime suspect.
Here’s what to keep an eye on:
- A runny nose that just won't stop, producing a thin, clear discharge.
- Lots of sneezing, even when they aren't cold.
- Eyes that are red, watery, and clearly itchy.
- A nagging, dry cough or little throat-clearing sounds.
Digestive System Distress
When a food is the culprit, the gut is often ground zero for the reaction. This can be tricky because most babies have some degree of gassiness or spit-up. With an allergy, these symptoms are usually more severe, consistent, and tied to feedings.
What many parents chalk up to "fussiness" can actually be a reaction to something like cow's milk protein, which is very different from lactose intolerance. You can learn more by reading our guide on the differences between baby lactose intolerance vs protein sensitivity.
Be on the lookout for these digestive red flags:
- Vomiting (not just gentle spit-up).
- Diarrhea or finding mucus in their diaper.
- Obvious pain, intense gas, or colic-like screaming that ramps up after eating.
- Suddenly refusing the breast or bottle, or pulling away in discomfort mid-feed.
There's no question that the need for safe allergy medicine for infants is on the rise. The global market for allergy treatments was valued at $21.7 billion in 2022 and is projected to skyrocket by 2032, a clear sign of how common these conditions are becoming in our kids.
Navigating Over-The-Counter Allergy Medicines
Staring at the pharmacy shelves filled with options for allergy medicine for infants can be completely overwhelming. You want to make the right choice for your little one, but it feels like a high-stakes decision. This is where knowing exactly what you're looking for becomes your best defense.
The world of allergy relief has come a long way. Not too long ago, the only options were first-generation antihistamines. Think of them as a heavy, old-fashioned blanket—they did the job, but they often came with a major side effect: drowsiness.
Today, pediatricians almost universally recommend the newer, second-generation antihistamines. These modern medications are far more targeted, blocking the allergic response without making your baby feel groggy. That’s a huge win for infants, who need to be alert and engaged to learn and grow.
Second-Generation Antihistamines: The Smarter Choice
When you’re reading the boxes, the key ingredients to look for are cetirizine (the active ingredient in Zyrtec) and loratadine (found in Claritin). These are the mainstays of the second-generation category and are often what doctors suggest first.
Think of an allergic reaction like a faulty alarm system in your baby's body. A harmless substance like pollen gets in, and the immune system mistakenly pulls the fire alarm, flooding the system with chemicals called histamines.
- First-generation antihistamines are like a clumsy worker who shuts down the entire power grid to stop the alarm. It works, but it makes everything else sluggish and sleepy.
- Second-generation antihistamines are more like a skilled technician. They go right to the source and disable the specific histamine alarm without causing that widespread drowsiness. Your baby feels better but can still be their normal, curious self.
This precision is exactly why these newer options are the go-to for infants who are old enough for medication.
There's one rule you absolutely cannot break: Never give any medication to an infant under six months old without explicit direction from a pediatrician. Even for older babies, that conversation with your doctor is non-negotiable.
Decoding the Label: What to Look For
Once your pediatrician gives you the green light, your next job is to become a label expert. Just because two boxes contain the same active ingredient doesn't mean the products are identical.
Here’s what you need to zero in on:
- Age and Formulation: Make sure the product is specifically made for infants or children. These usually come in liquid drops or syrups, which are much easier and safer to dose than trying to cut up an adult pill.
- Active Ingredients: Double-check that you're getting the second-generation antihistamine your doctor recommended (like cetirizine). Steer clear of "multi-symptom" formulas that pack in extra drugs like decongestants, as those aren't typically recommended for babies.
- Inactive Ingredients: Do a quick scan of everything else in the formula. Try to find products free from unnecessary dyes, sugars, or alcohol that could irritate your baby’s sensitive system.
The growing number of options reflects a big shift in how we manage allergies. The global allergy and sinus medicine market is valued at around $15 billion as of 2025 and is expected to keep growing, largely because parents want accessible, over-the-counter solutions. You can dive deeper into this trend and read the full research about the allergy medicine market.
Important Considerations for Caregivers
Even with the right medicine, your role as a caregiver is critical. If you're a breastfeeding mom, it's worth knowing that what you eat can sometimes affect your baby. Proteins from common allergens can pass through breast milk and cause a reaction in a sensitive infant. If you suspect that’s happening, your pediatrician can help you figure out the next steps. For more on this, check out our detailed guide on managing allergies while breastfeeding.
In the end, choosing an OTC allergy medicine for infants is a decision you make with your doctor, not for them. By understanding the real differences between medications and learning how to read labels like a pro, you can walk into that conversation feeling confident you're getting your baby the safest, most effective relief possible.
When Your Infant Needs a Prescription
Sometimes, over-the-counter allergy medicines just don't cut it. When you've tried the usual suspects and your baby is still fussy, itchy, or congested, it's not a failure on your part. It’s simply a cue to bring in your pediatrician for a more targeted approach. This is where prescription medications become an invaluable next step.
Thinking about prescriptions can feel a little intimidating for any parent, but it’s really about precision. A prescription isn’t a last resort; it’s a solution tailored specifically for your baby's age, weight, and symptoms when the standard options aren’t providing enough relief. This is especially true if allergies are starting to disrupt sleep, feeding, or just their general happy-go-lucky mood.
Stronger and More Targeted Antihistamines
While the newer OTC antihistamines work wonders for many babies, some little ones need something with a bit more oomph or a different mechanism. In these cases, a pediatrician might prescribe a more potent antihistamine or one specifically approved for younger infants.
This often comes into play when hives are particularly bad or when stuffiness is so constant that it’s making it hard for your baby to eat or sleep peacefully. Your doctor has access to a much wider toolkit of medications and precise dosing guidelines, letting them pick the exact right medicine for your child.
A prescription isn’t a red flag that something is terribly wrong. Think of it as your pediatrician fine-tuning the treatment plan, using their expertise to get your baby the most effective relief in the safest way possible.
Specialized Treatments for Skin and Nasal Issues
Allergies aren't always about sneezes and sniffles. For many babies, the real battle is happening on their skin or inside their tiny nasal passages.
- Steroid Nasal Sprays: When an oral antihistamine can't tame relentless congestion, your doctor might prescribe a very gentle, low-dose steroid nasal spray. These are lifesavers because they work directly on the inflamed tissue, calming the irritation right at the source.
- Prescription Creams for Eczema: If your baby’s eczema is severe, cracked, or just not getting better with over-the-counter hydrocortisone, it’s time for something stronger. A prescription topical steroid or a non-steroidal cream can finally break that miserable itch-scratch cycle and give their delicate skin a chance to heal.
The Crucial Role of an Epinephrine Auto-Injector
For infants diagnosed with a severe food allergy, a prescription becomes a life-saving tool. If your baby is at risk for anaphylaxis—a rapid, life-threatening allergic reaction—your pediatrician or allergist will prescribe an epinephrine auto-injector, such as an EpiPen Jr. or Auvi-Q.
This isn't for treating everyday sniffles. It's an emergency rescue device. Your specialist will walk you through a clear action plan, showing you exactly when and how to use it. Having one on hand provides critical peace of mind, ensuring you're ready to act immediately if the worst happens.
The entire field of pediatric healthcare is advancing to meet these challenges. The market for children's health solutions, including allergy treatments, was valued at $14.55 billion in 2024 and is projected to more than double by 2034. This surge is fueled by better diagnostic tools and a much deeper understanding of childhood allergies. You can explore more about the pediatric healthcare market and its growth on Precedenceresearch.com.
How to Give Medicine to Your Baby Safely
Trying to give medicine to a squirming, unhappy baby can feel more like a wrestling match than a simple task. But getting it right is crucial for their safety and comfort. The single most important rule to burn into your memory is that infant dosing is always based on weight, not age. A baby’s tiny, still-developing body metabolizes medicine very differently, and what might be a safe dose for a chunky six-month-old could be dangerous for a smaller one of the same age.
This is exactly why reaching for a regular kitchen spoon is one of the biggest mistakes a parent can make. Teaspoons and tablespoons vary wildly in size—some hold nearly twice as much as others. That’s a level of guesswork you just can’t afford when it comes to allergy medicine for infants.
Mastering the Oral Syringe
The best tool for the job is the humble oral syringe—that small, plastic dispenser that often comes with liquid medicine or is available at any pharmacy. It lets you measure a precise dose down to the milliliter, taking all the guesswork out of the equation.
Here’s how to make the process as smooth as possible:
- Read the Label First: Before you even open the bottle, double-check the label and your doctor's instructions. Confirm the exact dose in milliliters (mL).
- Draw Up the Medicine: Place the tip of the syringe into the medicine and slowly pull the plunger back until you hit the correct measurement line. Flick the syringe to get rid of any large air bubbles.
- Get Your Baby in Position: Hold your baby securely in a semi-upright position, much like you would for a feeding. Never try to give medicine while they're lying flat on their back, as this is a serious choking hazard.
- Aim for the Cheek Pouch: This is the game-changing tip. Don't squirt the medicine straight down their throat, which will almost always trigger a gag reflex. Instead, gently slip the syringe into their mouth between the gums and the inside of their cheek.
- Go Slow and Steady: Push the plunger down gradually, giving your baby a moment to swallow each little bit. This simple trick makes it much less likely they'll spit the whole dose right back at you.
Sometimes, even with your best efforts, over-the-counter options just aren't cutting it. If you find yourself in that boat, it’s time to talk to your pediatrician about prescription options.
Moving to a prescription isn't a sign of failure; it's the logical next step you take with your doctor to find a more targeted solution for your little one's symptoms.
Critical Safety Do's and Don'ts
Beyond just getting the medicine in, a few non-negotiable rules are essential for keeping your baby safe. Following these guidelines helps protect them from accidental overdoses or dangerous interactions.
Never mix medicine into a full bottle of formula or breast milk. If your baby doesn’t finish the bottle, you have no way of knowing how much of the dose they actually got.
To make things crystal clear, here’s a quick-reference table that covers the most important practices.
Safe Medication Practices Do's and Don'ts
This table breaks down the safe way to handle infant medication versus common—and potentially dangerous—mistakes.
| Action | Do (The Safe Way) | Don't (The Unsafe Way) |
|---|---|---|
| Dosing Tool | Use the oral syringe or dropper that came with the medicine for accurate mL measurements. | Never use a kitchen spoon, which can lead to significant under- or overdosing. |
| Medication Type | Only use products specifically formulated for infants or children, as directed by your doctor. | Avoid giving adult medications or "multi-symptom" cold remedies unless explicitly told to. |
| Tracking Doses | Keep a simple log of what medicine you gave and at what time to prevent accidental double-dosing. | Never guess when the last dose was given, especially when multiple caregivers are involved. |
| Consulting a Pro | Always check with your pediatrician or pharmacist before combining any medications. | Don't mix different allergy treatments or other drugs without getting medical approval first. |
Sticking to these best practices ensures that every dose of allergy medicine for infants is not only effective but, more importantly, completely safe.
Everyday Strategies for Allergy Relief at Home
While the right allergy medicine for infants is a game-changer, it’s really just one piece of the puzzle. The most effective approach involves creating an allergy-friendly home environment. Think of it as building a protective bubble around your baby, one that minimizes their contact with the very things triggering their symptoms.
You don't need to overhaul your entire house. Small, consistent habits can make a world of difference in your little one's daily comfort by making your home an unwelcome place for tiny irritants like dust, pollen, and dander.
Creating a Low-Allergen Nursery
Your baby’s nursery should be their safe haven. With a few simple tweaks, you can turn it into a low-allergen zone where they can rest and breathe easier.
- Purify the Air: A good high-efficiency particulate air (HEPA) filter is your best friend here. It works quietly to trap airborne allergens like pollen, pet dander, and dust mites. Running one in the nursery, especially overnight, can significantly clear the air your baby breathes.
- Wash Bedding Hot: Dust mites are a huge trigger for indoor allergies. The best way to get rid of them is to wash all crib bedding—sheets, mattress pads, everything—in hot water (at least 130°F or 54°C) at least once a week.
- Establish a Pet-Free Zone: We know they're part of the family, but if pet dander is the problem, keeping furry friends out of the nursery is crucial. This simple boundary gives your baby a solid eight-plus hours of allergen-free breathing space every single night.
For parents exploring additional non-medicinal ways to create a comforting atmosphere, using a portable nebuliser for home fragrance and air humidification can help maintain a soothing environment.
Soothing Sensitive Skin
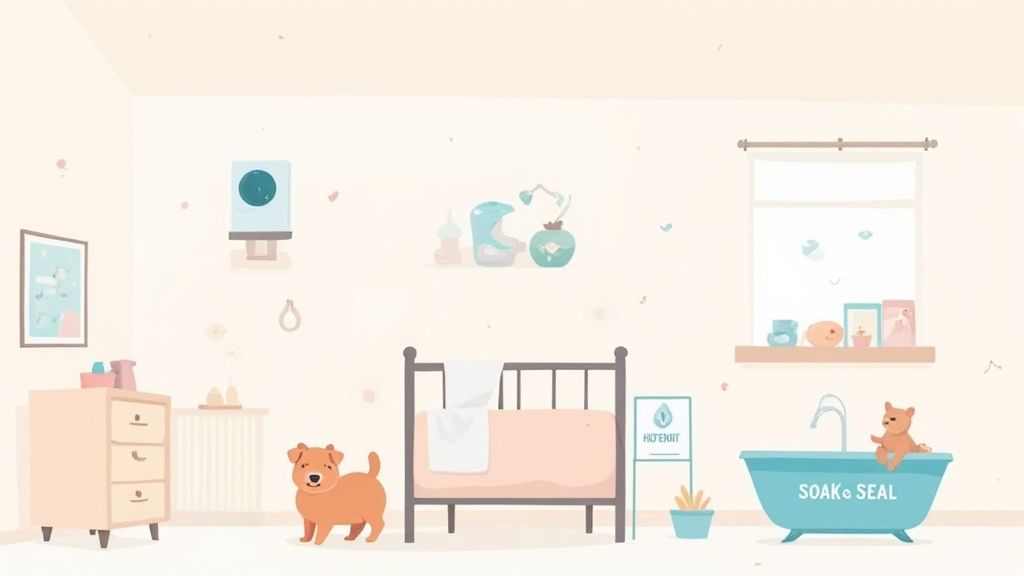
When you're dealing with skin allergies like eczema, what you do around your baby is just as important as what you put on their skin. The name of the game is protecting and hydrating their incredibly delicate skin barrier.
Dermatologists often recommend the "soak and seal" method, and it's as powerful as it is simple. First, give your baby a short, lukewarm bath (just 5-10 minutes) with a gentle, fragrance-free cleanser. Then, immediately after patting them dry—while their skin is still a bit damp—you "seal" in that hydration with a thick, generous layer of fragrance-free cream or ointment.
This bath routine is more than just getting clean; it's a therapeutic treatment. The soak delivers moisture deep into the skin, and the seal creates a protective layer that locks it in and keeps irritants out. This can be key to breaking the miserable itch-scratch cycle.
A consistent skincare routine is everything. For more detailed advice, check out our complete guide on baby skin care 101 for new parents.
The Role of a Breastfeeding Diet
If you're breastfeeding a baby with suspected allergies, it’s good to know that tiny proteins from the foods you eat can pass into your breast milk. In some sensitive infants, these proteins can trigger a reaction. The most common offenders are cow's milk protein, soy, eggs, and nuts.
Should your pediatrician suspect a food allergy is at play, they might suggest a temporary elimination diet. This means you'll remove a potential trigger food from your diet for a couple of weeks to see if your baby's symptoms get better. It’s critical that this is always done under medical supervision to ensure both you and your baby continue to get all the nutrients you need to thrive.
Knowing the Red Flags for an Allergic Reaction
Most of the time, allergy symptoms are mild and can be managed with help from your pediatrician. But it's critical to know the difference between a minor reaction and a severe one.
A severe, life-threatening allergic reaction is called anaphylaxis. It’s a true medical emergency that can happen within seconds or minutes of your baby being exposed to an allergen, and it requires immediate action.
Knowing what to look for isn't about being scared—it's about being prepared. When you can spot these red flags, you can act quickly and confidently. This is probably the most important part of your allergy toolkit.
Immediate Emergency Signs
If you see any of the symptoms below, especially right after your baby tries a new food or comes into contact with a known allergen, call 911 immediately. Don't wait to see if things get better on their own.
- Difficulty Breathing: Look for wheezing, a hoarse cry, a persistent cough, or fast, shallow breaths. You might also notice the skin around their ribs or neck sucking in as they struggle to breathe.
- Swelling of the Face: Pay close attention to any sudden puffiness around the lips, tongue, or eyes.
- Widespread Hives: A few hives here and there are one thing. But a sudden rash of hives covering large areas of their body is a major warning sign.
- Sudden Lethargy or "Floppiness": If your baby suddenly goes limp, becomes unresponsive, or seems unusually drowsy, it's a critical sign.
- Vomiting or Severe Diarrhea: This is especially concerning when it happens along with any of the other symptoms on this list.
Trust your gut. If you feel like something is seriously wrong with your baby, it probably is. Never hesitate to get emergency help. It is always, always better to be safe than sorry.
Recognizing these signals is a key part of being prepared for any emergency. To round out your knowledge, our guide on baby first aid basics every parent should know is a great resource. Acting fast can make all the difference.
Answering Your Top Questions About Infant Allergies
Even after a helpful chat with your pediatrician, questions about your baby's allergies can pop up at the most inconvenient times. You might remember something you forgot to ask or just need a quick refresher. That's what this section is for.
Think of this as your go-to reference for those middle-of-the-night worries. We'll walk through some of the most common concerns parents have when navigating allergy medicine and symptoms for their little ones.
Can I Give My Infant Benadryl?
This is a big one. Most pediatricians strongly advise against giving Benadryl (diphenhydramine) to infants unless they've specifically told you to. Benadryl is an older, first-generation antihistamine, and it can hit a baby's system pretty hard.
The side effects can be unpredictable—some babies become extremely drowsy, while others have the complete opposite reaction and become hyperactive. Newer, second-generation antihistamines are much safer and are the preferred choice for infants. The bottom line is to always, always check with your doctor before giving your baby any kind of antihistamine.
How Do I Know if It Is Allergies or Just a Cold?
It’s genuinely tough to tell the difference at first glance since the symptoms look so similar. One of the biggest giveaways is a fever. Colds often bring a low-grade fever with them, but allergic reactions almost never do. That's a major clue.
Another thing to look at is the mucus. It's not glamorous, but it's helpful!
- Cold Mucus: Usually starts clear but often becomes thick and can turn yellow or even green as the cold progresses.
- Allergy Mucus: Tends to stay clear, thin, and watery.
Finally, think about timing. A cold typically clears up in about a week. Allergy symptoms, on the other hand, can drag on for weeks or even months if your baby is constantly exposed to the trigger.
The rule of thumb is simple: If you're seeing cold-like symptoms that just won't quit after a couple of weeks, and there's no fever, it’s a good time to call the pediatrician to discuss allergies.
If I Breastfeed, Can My Diet Affect My Baby's Allergies?
Yes, absolutely. This is a crucial connection for breastfeeding moms to understand. Tiny proteins from the foods you eat can pass through to your breast milk. If your baby has a food allergy to something like cow's milk, soy, or eggs, they can react to your milk after you've eaten those foods.
If your doctor suspects a food allergy, they might suggest trying an elimination diet. This means you'll temporarily remove a common trigger food from your diet to see if your baby's symptoms get better. This should only be done with professional medical guidance to make sure both you and your little one are getting all the nutrients you need. For more on this topic, check out our guide on Allegra and breastfeeding.
At MoogCo, we know that being a mom is full of questions. Our Original Silver Nursing Cups are here to offer a simple, natural solution for one of breastfeeding's biggest challenges. They provide soothing relief and protection, letting you focus on your baby. Discover a chemical-free way to find comfort by exploring our silver nursing cups on Amazon.