Pregnancy nausea, or "morning sickness" as it's often called, is one of the most common—and frankly, most talked about—parts of early pregnancy. It’s a direct response to the incredible hormonal tidal wave that kicks off a healthy pregnancy.
Think of it this way: your body is installing a powerful new operating system to grow a baby. This surge in hormones, especially hCG, can temporarily throw your system off balance, leading to that all-too-familiar queasy feeling. While it can certainly feel miserable in the moment, it’s often a reassuring sign that things are progressing just as they should.
Why Nausea Is So Normal in Pregnancy

If you’re dealing with nausea and vomiting during pregnancy (often abbreviated NVP), you are in very good company. It's so incredibly common that it's practically a universal part of the experience for most expecting mothers.
Just how widespread is it? A massive analysis that pulled together data from 59 different studies found that nausea and vomiting affect roughly 69.4% of pregnant women around the globe. That review covered over 93,000 people, giving us a really solid picture of what to expect. Knowing you're part of such a huge group can be a small comfort on tough days.
The Spectrum of "Morning Sickness"
The term "morning sickness" is a bit of a misnomer, as anyone who has felt queasy at dinnertime can tell you. The discomfort can show up at any time of day or night. It’s also not a one-size-fits-all experience; it exists on a spectrum from mild, fleeting queasiness to something far more persistent.
Here’s how the global data generally breaks down for those with NVP:
- Mild Symptoms: About 40% of women experience this level.
- Moderate Symptoms: A slightly larger group, around 46%, falls into this category.
- Severe Symptoms: A smaller but still significant 14% deal with more intense symptoms.
For most women, the worst of it is concentrated in the early weeks. Getting through this period is a major milestone, and we've put together some helpful tips in our complete first trimester guide. It’s also worth knowing that for about 23.5% of women, NVP can linger into the third trimester, requiring a bit more management.
The key takeaway is that your experience, whether it's a bit of queasiness or more moderate nausea, is a normal physiological response. It’s your body working hard, not a sign that something is wrong.
When Nausea Crosses the Line
While most NVP is manageable, there's a much more severe condition called hyperemesis gravidarum (HG). This is not typical morning sickness. It's a relentless and debilitating condition that affects a much smaller fraction of pregnancies, with a global prevalence of around 1.1%.
Unlike standard NVP, HG involves severe and persistent vomiting that poses real health risks. The warning signs include:
- Significant weight loss (losing more than 5% of your pre-pregnancy weight)
- Severe dehydration that you can't correct by drinking fluids
- Electrolyte imbalances
If typical morning sickness is a bumpy road, HG is a relentless storm that requires immediate medical help. Knowing the difference is so important—it empowers you to see when your symptoms have gone from being a difficult part of pregnancy to a potential danger, so you can get the care you and your baby need right away.
Lifestyle and Diet Changes to Manage Nausea

Before we even get to discussing an anti nausea medicine pregnancy might call for, it’s worth starting with the basics. Many people find incredible relief just by tweaking their daily routines and eating habits. These simple, safe strategies are always the first line of defense and can often reduce nausea so much that medication isn't even necessary.
Think of an empty stomach as a tinderbox. When it’s empty, stomach acid builds up and blood sugar plummets, creating the perfect recipe for a sudden wave of queasiness. The goal is to avoid this scenario altogether.
There's a good reason why keeping crackers on your nightstand is classic advice. Nibbling on a few simple carbs before you even lift your head off the pillow can help absorb that stomach acid and stabilize your blood sugar, setting a much calmer tone for the day.
Rethink Your Meal Schedule
The standard three-square-meals-a-day plan? It just doesn't fly for most people in early pregnancy. A stomach that’s too full can be just as much of a trigger as one that’s empty. The real secret is to become a grazer.
Try to eat small, frequent meals or snacks every 1.5 to 2 hours. This approach keeps your blood sugar from crashing and ensures your stomach is never completely empty or uncomfortably stuffed—the two biggest culprits behind nausea.
A day of eating might look something like this:
- 7:00 AM: A few dry crackers before you get out of bed.
- 8:30 AM: A small piece of toast or a little bowl of oatmeal.
- 10:30 AM: An apple and a handful of almonds.
- 12:30 PM: Half a sandwich and a cup of yogurt.
- 3:00 PM: A cheese stick and some grapes.
- 5:30 PM: A small serving of chicken with rice and steamed veggies.
- 8:00 PM: A cup of yogurt or a simple smoothie.
Making these simple dietary shifts, along with maintaining healthy eating habits, can make a world of difference in how you feel.
Choose Your Foods and Fluids Wisely
What you eat is just as important as when you eat it. During these early weeks, some foods will be your best friends, while others might feel like your worst enemies.
Generally, foods that are bland, high in carbs, and low in fat are the easiest to digest and tolerate.
Here are a few good options to lean on:
- Bland Carbs: Think crackers, plain toast, pretzels, rice, and pasta.
- Lean Proteins: Baked chicken or fish and beans are often good choices.
- Simple Fruits: Bananas, applesauce, and melons are usually well-received.
- Soothing Liquids: Clear broths, weak teas, and electrolyte drinks can be comforting.
For many, sipping on a thoughtfully chosen beverage can bring a lot of comfort. If you need some ideas, check out our guide to the best anti-nausea tea for pregnancy.
A crucial mindset shift is to focus on what you can eat instead of what you can't. Don't stress about a perfectly balanced diet right now; the main goal is to stay hydrated and keep some calories down.
On the flip side, some foods are notorious for triggering nausea. Fatty, greasy, spicy, or very acidic foods are often the problem. You might want to take a temporary break from things like fried foods, heavy sauces, and even citrus until your stomach settles down.
Minimize Sensory Overload
During pregnancy, your sense of smell can become almost superhuman. Scents you once loved or hardly noticed can suddenly become overpowering and bring on a bout of sickness.
Figuring out your personal scent triggers and avoiding them is a powerful move. This might mean:
- Steering clear of the kitchen while someone else is cooking.
- Choosing cold or room-temperature foods, which have far less aroma than hot dishes.
- Asking your partner to skip the strong cologne or perfume for a while.
- Keeping windows open for fresh air and good ventilation.
Finally, never underestimate the power of rest. Being exhausted makes nausea so much worse. Prioritizing naps and getting a full night's sleep gives your body the resources it needs to handle all the incredible changes happening. These simple adjustments really do form the foundation for managing nausea.
Finding Safe Over-The-Counter Relief
When sipping bland broth and nibbling crackers just isn't enough, your next stop is likely the pharmacy aisle. The good news is that some of the most effective and well-studied remedies for an anti nausea medicine pregnancy requires are available right over the counter. These aren't just old wives' tales; they are the evidence-based, first-line treatments that doctors recommend every day.
The whole point is to find something that works for you without posing any risk to your growing baby. Let's walk through the most trusted OTC solutions, starting with the gold-standard combination that has brought relief to countless pregnant people.
The Power Duo: Vitamin B6 and Doxylamine
One of the most effective treatments for nausea and vomiting during pregnancy is the simple combination of Vitamin B6 (pyridoxine) and doxylamine. This pairing is so reliable that it’s the active ingredient in the prescription drug Diclegis. But you don't have to wait for a prescription to get the benefits of these two components.
Think of them as a tag team. Vitamin B6 is the main player, helping to quell those awful nausea signals. Doxylamine, which is an antihistamine you might recognize from sleep aids like Unisom SleepTabs, adds another layer of anti-nausea power and can be a huge help when queasiness keeps you up at night.
This combo isn't new; it's been used safely for decades. The FDA gives it a Category A rating, meaning that high-quality studies have shown no risk to the fetus, even in the first trimester.
Many doctors suggest starting slow. You can begin with just Vitamin B6 and then add doxylamine later if you find you need more help, especially for that dreaded middle-of-the-night nausea.
How to Dose Vitamin B6 and Doxylamine Correctly
Getting the dose right is everything. It's always best to chat with your doctor or midwife before starting anything new, but a very common approach looks like this:
- Step 1: Start with Vitamin B6. Begin by taking 10 to 25 mg of Vitamin B6 (pyridoxine) up to three times a day. Taking it with a small meal can help.
- Step 2: Add Doxylamine for Nighttime Relief. If you're still struggling, especially at night, try adding half of a 25 mg doxylamine tablet (12.5 mg) before bed. The mild drowsiness is often a welcome side effect.
- Step 3: Combine for All-Day Coverage. If you need more comprehensive relief, your provider can help you figure out a schedule that involves taking both during the day.
This tiered approach lets you customize the treatment to your own needs, ensuring you're using the lowest dose that still works. And don't forget—your prenatal vitamin already has some Vitamin B6 in it. It's worth knowing what's in your daily multi, so you might want to learn more about if Nature Made prenatal vitamins are good and what ingredients matter most.
Ginger: A Natural and Proven Alternative
If you'd rather start with a natural remedy, ginger is a fantastic, research-backed option for taming pregnancy nausea. This is one folk remedy that modern science actually supports.
Ginger is believed to work by calming the stomach and the entire digestive tract. Its active compounds, called gingerols and shogaols, have properties that can gently but effectively soothe that queasy feeling. Best of all, it comes in so many forms.
Here are a few easy ways to work ginger into your day:
- Ginger Capsules: For a precise and consistent dose, supplements are a great option. A typical recommendation is 250 mg, taken up to four times a day.
- Ginger Tea: There's nothing quite like sipping on warm ginger tea. You can buy pre-made tea bags or just steep a few slices of fresh ginger root in hot water.
- Ginger Candies or Chews: These are perfect for stashing in your bag for nausea emergencies. Sucking on a crystallized ginger chew can stop a wave of queasiness in its tracks.
- Ginger Ale: Just make sure you grab a brand made with real ginger, not just artificial flavoring. Letting it go a little flat can sometimes make it even easier to stomach.
Comparing First-Line OTC Anti-Nausea Options
To help you see the options side-by-side, here’s a quick breakdown of the most common over-the-counter and natural remedies for morning sickness. This table summarizes how they work, their typical dosages, and key things to keep in mind.
| Treatment | How It Works | Common Dosage | Key Considerations |
|---|---|---|---|
| Vitamin B6 (Pyridoxine) | Believed to help regulate neurotransmitters involved in nausea signals. | 10-25 mg, 3-4 times per day. | Often the first step. Can be taken alone or with doxylamine. Check your prenatal vitamin for total daily intake. |
| Doxylamine Succinate | An antihistamine that blocks certain receptors in the brain to reduce nausea. | 12.5 mg (half a 25 mg tablet), 1-2 times per day, often at night. | Very effective, especially when combined with B6. Causes drowsiness, making it ideal for bedtime use. |
| Ginger (Capsules, Tea, Chews) | Contains compounds like gingerols that have anti-nausea and anti-inflammatory effects on the digestive system. | Up to 1,000 mg per day, often split into doses of 250 mg. | A natural, evidence-based option. Some people find it can cause mild heartburn. |
Ultimately, whether you choose the potent duo of B6 and doxylamine or the natural comfort of ginger, these OTC solutions offer safe, accessible ways to get a handle on your symptoms. They put the power back in your hands, helping make this part of your pregnancy journey a whole lot more comfortable.
When Prescription Anti-Nausea Medicine Is Necessary
So you’ve tried the diet tweaks, the ginger, and the Vitamin B6/doxylamine combo, but the nausea just isn't letting up. What's next? This is the point where it's time to have a different kind of conversation with your doctor.
For anyone wrestling with moderate to severe morning sickness, prescription anti-nausea medication isn't just a convenience—it's often a crucial tool for keeping you and your baby healthy.
Taking that step to a prescription can feel significant, but it's a very common and often necessary part of managing persistent nausea and vomiting. The main goal here is simple: to prevent the serious one-two punch of dehydration and malnutrition. When you can’t keep anything down, your body isn't getting the fuel it needs to function, let alone to support a growing baby.
The path to managing nausea usually starts with the basics, as this chart shows.
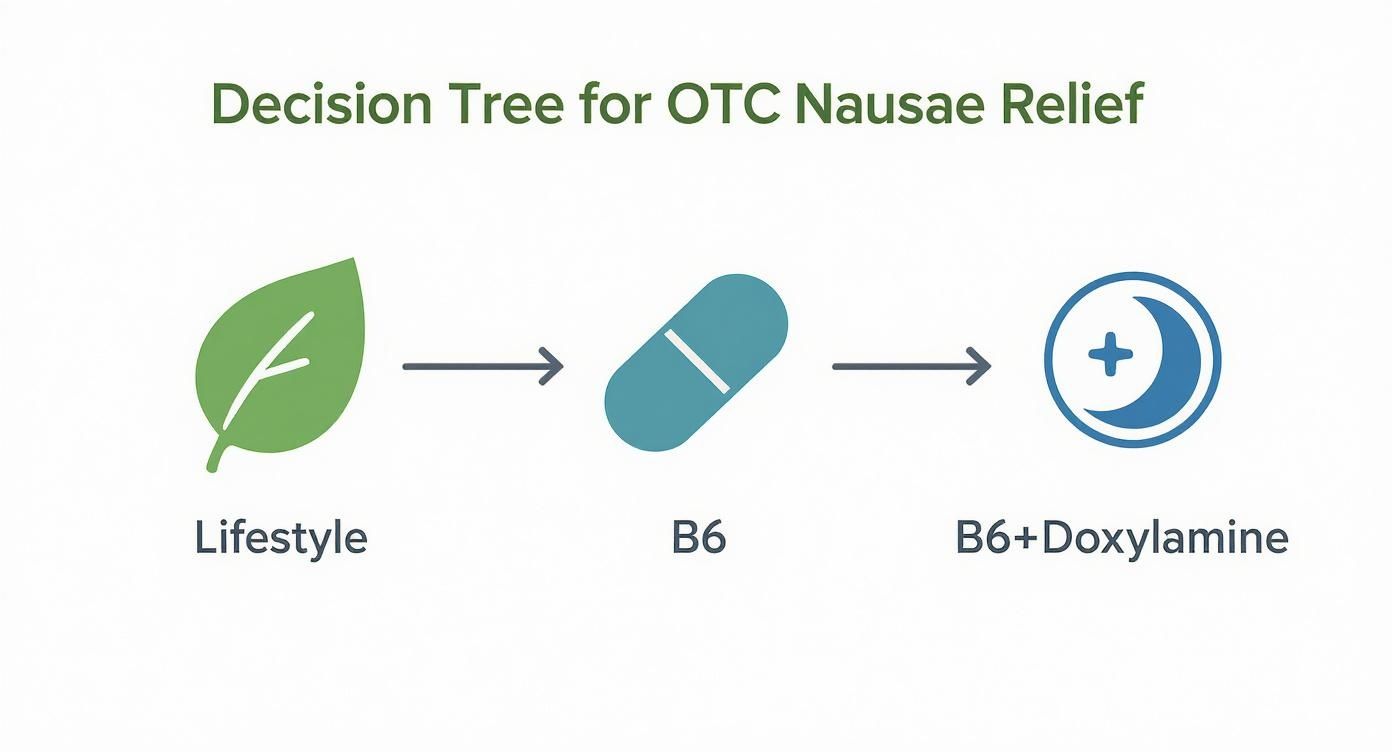
When these first-line approaches aren't enough to get you through the day, your provider will start considering the prescription options we'll get into below.
Common Prescription Medications for Nausea
If your doctor decides a stronger approach is needed, they have several well-researched medications in their toolkit. Each one works a bit differently to get nausea and vomiting under control. Let's look at three of the most common ones.
Metoclopramide (Reglan)
Metoclopramide works by encouraging your stomach to empty faster, moving food into the intestines more quickly. It also directly affects the nausea center in your brain. By keeping things moving in the right direction, it helps reduce the chances that anything will come back up.
This is often a go-to second-line treatment. A key side effect to be aware of is drowsiness, so you'll want to see how it affects you before you get behind the wheel.
Promethazine (Phenergan)
Promethazine is an antihistamine with some serious anti-nausea power. It works by blocking brain signals that trigger the vomiting reflex. While it's very effective, it's also famous for causing significant drowsiness.
Because it can make you so sleepy, doctors often suggest taking it at night. This way, it can help you get some much-needed rest while also keeping nausea from waking you up.
The risk-versus-benefit conversation with your doctor is everything. For most, the very real risk of dehydration from uncontrolled vomiting is a much bigger threat than the potential side effects of a well-studied medication. Your doctor’s recommendation is always aimed at keeping both you and your baby safe.
A Closer Look at Ondansetron (Zofran)
Ondansetron, which most people know by the brand name Zofran, is another incredibly effective and widely used medication for nausea during pregnancy. It’s part of a class of drugs called serotonin 5-HT3 receptor antagonists. Fun fact: it was first developed to help cancer patients deal with nausea from chemotherapy. It works by blocking serotonin, a chemical in the body that can trigger intense nausea and vomiting.
For years, Zofran has been a lifesaver for those with severe morning sickness that just won't quit. For many, it's the one thing that finally allows them to eat, drink, and get back to their lives.
Discussing the Safety of Zofran
The conversation around Zofran has become more complex over the years, especially regarding its use in the first trimester. You may have seen headlines about conflicting studies—some suggesting a very small potential increase in the risk of certain birth defects, while other massive studies have found no significant risk at all. This has understandably created a lot of confusion and anxiety.
Ondansetron was the top anti-nausea drug prescribed in the U.S. from 2000 to 2014, used in roughly 15.2% of pregnancies. Despite how common it is, the conflicting data has led some health organizations to recommend against using it as a first choice during the first trimester.
So, what’s the bottom line? Here’s what the current medical consensus generally looks like:
- The Absolute Risk is Tiny: Even in the studies that found a possible link, the actual increase in risk for things like heart defects or cleft palate was incredibly small—we're talking fractions of a percent.
- Benefits Often Outweigh the Risks: For someone heading toward hyperemesis gravidarum, the dangers of severe dehydration and weight loss are immediate and serious. In these situations, an effective medication like Zofran is often considered far more beneficial than the very small potential risk.
- A Second-Line Choice: Because of this ongoing discussion, most doctors now save Zofran for cases where first-line treatments (like the B6 and doxylamine combo) just haven't worked.
It’s completely normal to feel anxious when you hear about any potential risk. This is why having a candid talk with your provider is so critical. They can help put the data into perspective for your specific health situation. For a broader look at what to expect at different stages, check out our guide on navigating pregnancy at frequent intervals.
Ultimately, deciding to use a prescription anti-nausea medicine is a team decision. It's about looking at the evidence together, understanding what you need, and choosing the path that best protects both your health and your baby's.
When Morning Sickness Becomes Something More: Hyperemesis Gravidarum
While most women experience some level of nausea during pregnancy, there's a much more severe condition called hyperemesis gravidarum (HG). This isn't just "bad morning sickness." It's a debilitating medical diagnosis that requires professional care. HG represents the most extreme end of the nausea and vomiting spectrum, affecting an estimated 0.3% to 3% of pregnancies.
Think of it this way: if typical morning sickness is like dealing with a bit of seasickness on a choppy day, hyperemesis gravidarum is like being caught in a relentless hurricane. The constant, severe nausea and vomiting can completely sideline you, making it impossible to go about your daily life. Unlike standard nausea, HG can lead to serious health issues for the mother if it's not managed properly.
Is It Morning Sickness or HG?
So, how can you tell when you’ve crossed the line from manageable nausea into something more serious? The distinction isn't just about feeling extra sick. Your doctor will look for very specific clinical signs that show the condition is taking a significant physical toll.
The main signs that point to a diagnosis of HG include:
- Serious Weight Loss: A key red flag is losing more than 5% of your pre-pregnancy body weight because you simply can't keep food down.
- Persistent Dehydration: When you can't keep fluids down, your body becomes dehydrated. This shows up as dark urine, extreme weakness, dizziness, and dry skin.
- Electrolyte Imbalances: Constant vomiting disrupts the crucial balance of minerals like potassium and sodium in your body, which can be confirmed with blood tests.
The real difference is that with morning sickness, you can usually find something you can eat or drink and keep down. With HG, the vomiting is often relentless—sometimes more than three times a day—and it can feel like you can't tolerate anything by mouth at all.
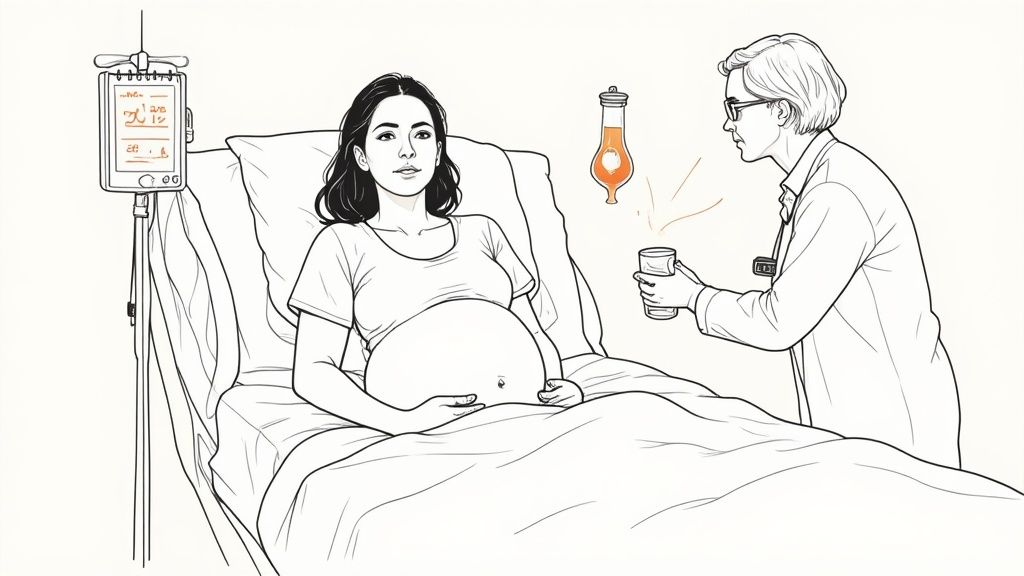
How Hyperemesis Gravidarum Is Treated
Because HG can lead to malnutrition and severe dehydration, the treatment plan is far more intensive than what's needed for typical nausea. The primary goals are to rehydrate you, restore nutrients, and get the vomiting under control.
This often means a hospital stay is necessary. Management strategies usually involve:
- Intravenous (IV) Fluids: This is the first-line treatment. Getting fluids, electrolytes, and vitamins directly into your bloodstream is the fastest way to correct dehydration and restore balance.
- IV Medications: If you can't keep oral pills down, anti-nausea medications are given through your IV for a much stronger and more immediate effect.
- Nutritional Support: In very severe cases, nutrition may need to be supplied through a feeding tube or even an IV line (a method called total parenteral nutrition, or TPN) to ensure you and your baby get essential nutrients.
- Careful Monitoring: In the hospital, your care team will keep a close eye on your weight, hydration levels, and labs to make sure both you and your baby are safe and stable.
It's crucial to know the signs of HG. If your nausea and vomiting are so constant that you're losing weight and can't stay hydrated, please contact your provider right away. This is not a condition you can just "tough out." It requires prompt, compassionate, and intensive medical support to keep you and your baby healthy.
A Partner's Guide to Providing Support
It’s tough watching someone you love struggle with pregnancy nausea, and it can leave you feeling completely helpless. But that feeling doesn't have to be the whole story. Your support is one of the most powerful tools she has, and you can turn that helplessness into real, practical action that makes a huge difference.
Your role here is part practical, part emotional, and part logistical. Simple things, like taking over in the kitchen to keep cooking smells at bay or making sure there's always a stash of crackers and ginger ale on hand, are massive wins. Being the one to run to the store for a weird food craving or a different anti nausea medicine pregnancy allows for can lift a heavy weight off her shoulders.
Practical and Emotional Backup
The physical drain of constant nausea is one thing, but the emotional toll is just as significant. The most important thing you can do is validate what she's going through. Instead of saying, "It's just morning sickness," try something like, "I'm so sorry you're feeling this awful. What can I do to help right now?" That small change shows you see her struggle and you're on her team.
You can also step in as her advocate and external hard drive.
- Track Symptoms: Help keep a simple log of what she eats, when the nausea hits hardest, and how she’s feeling. This kind of information is gold for her doctor.
- Manage Medications: Keep track of her medication schedule to make sure she doesn't miss a dose, especially when she’s feeling too sick to remember.
- Be Her Voice: During appointments, you can help share the details you've tracked and make sure all of her—and your—questions get answered.
Understanding the Bigger Picture
It also helps to understand a bit of the medical context. Pregnancy care has changed a lot over the years, and being an informed partner is a big deal. For example, a drug called Bendectin was prescribed to about 25% of pregnant women back in the 1960s and 70s. Decades later, it was linked to long-term health risks in their children, with studies connecting prenatal exposure to an increased risk of colorectal cancer. This is a powerful reminder of why careful medication management and clear communication with doctors are so crucial.
Providing steadfast support is about more than just managing symptoms; it’s about strengthening your partnership before the baby arrives. By taking on these supportive roles, you are actively participating in the pregnancy journey.
This kind of teamwork is incredible practice for what comes next. For more on how partners can keep up this vital support after birth, check out our guide on the role of fathers in the breastfeeding journey.
Common Questions About Nausea During Pregnancy
It's completely normal to have a lot of questions when you're trying to manage nausea during pregnancy. Getting clear answers is the first step toward feeling better and making informed choices with your doctor. Let's walk through some of the most common concerns.
Understandably, the biggest question is usually about safety. You can feel confident knowing that first-line treatments, like the combination of Vitamin B6 and doxylamine, are among the most studied medications in pregnancy. They have a long-standing safety record for both mom and baby.
When Is It Time to Call the Doctor?
While some level of nausea is a classic pregnancy symptom, it can sometimes cross the line into something more serious. Knowing the red flags is key.
You should get in touch with your provider if you:
- Can't keep any food or liquids down for 24 hours.
- Start losing weight.
- Feel dizzy, weak, or like you might faint when you stand up.
- See signs of dehydration, like very dark urine or not peeing often.
The most important thing to remember is that you don't just have to suffer through it. If nausea and vomiting are making it impossible to get through your day, that is more than enough reason to ask for help.
Another big question is, "Will this last forever?" For the vast majority of women, the worst of it fades away somewhere between weeks 12 and 14, right as the second trimester begins. A small number might have symptoms that linger, but for most, there's a light at the end of the tunnel.
At MoogCo, we understand the journey through pregnancy and into postpartum life. Our Original Silver Nursing Cups offer natural, soothing relief for breastfeeding mothers, helping you get a comfortable start. Find the chemical-free protection you and your baby deserve.