When you're pregnant, the to-do list can feel a million miles long. Between setting up the nursery and picking out a car seat, it's easy to put breastfeeding on the back burner. But taking a little time to prepare before your baby arrives can honestly be a game-changer. It’s one of the best things you can do to build your confidence and set yourself up for a smoother start.
The goal isn't perfection—far from it. It's about arming yourself with knowledge, getting your supplies ready, and, most importantly, building a solid support system. Doing this work now helps turn those potential "what do I do?!" moments into manageable, expected steps.
Building Your Breastfeeding Confidence Before Birth
Let’s be real: thinking about breastfeeding before your baby is even in your arms can feel abstract and a little intimidating. Many new parents feel this way. But a bit of proactive learning can make all the difference, shifting your experience from stressful to successful.
This early investment is incredibly powerful. It helps you understand what to expect—from your baby's hunger cues to your own body's signals—so you can navigate the early days feeling capable and in control.
Why Prenatal Preparation Matters
The research really backs this up. Early education on breastfeeding before you give birth has a huge impact on whether you start and for how long you continue. In the United States, for example, breastfeeding initiation rates jumped from 48.3% in 2002 to 83% by 2017, thanks in large part to better prenatal education and support.
But here’s the kicker: despite so many starting, only 35.9% were still breastfeeding at the one-year mark. This tells us that starting strong is just half the battle. A solid foundation built during pregnancy is what helps you stick with it through the challenges. Feeling prepared helps you troubleshoot a tricky latch or get through a long night of cluster feeding without feeling defeated.
For more hands-on advice, check out our quick-start guide with breastfeeding tips for first-time moms.
To help you get organized, I’ve put together a simple timeline to help you tackle your breastfeeding prep trimester by trimester. This way, you can spread things out and feel ready, not rushed.
Your Prenatal Breastfeeding Preparation Timeline
Here is a simple timeline to help you organize your breastfeeding preparation tasks by trimester so you feel ready and not rushed.
| Trimester | Key Focus Areas | Actionable Steps |
|---|---|---|
| First (Weeks 1-12) | Education & Mindset | • Read books/blogs • Discuss breastfeeding goals with your partner • Start a conversation with your OB/GYN or midwife |
| Second (Weeks 13-27) | Skill Building & Consultation | • Take a breastfeeding class • Schedule a prenatal consult with a lactation consultant (IBCLC) • Address any nipple or breast concerns |
| Third (Weeks 28-40+) | Planning & Logistics | • Create your breastfeeding plan for the hospital • Gather supplies (pump, bottles, nursing bras, Silverette cups) • Set up a "nursing station" at home |
This timeline helps break down what can feel like a huge task into smaller, more manageable pieces, moving from learning the basics to getting all your practical plans in place.
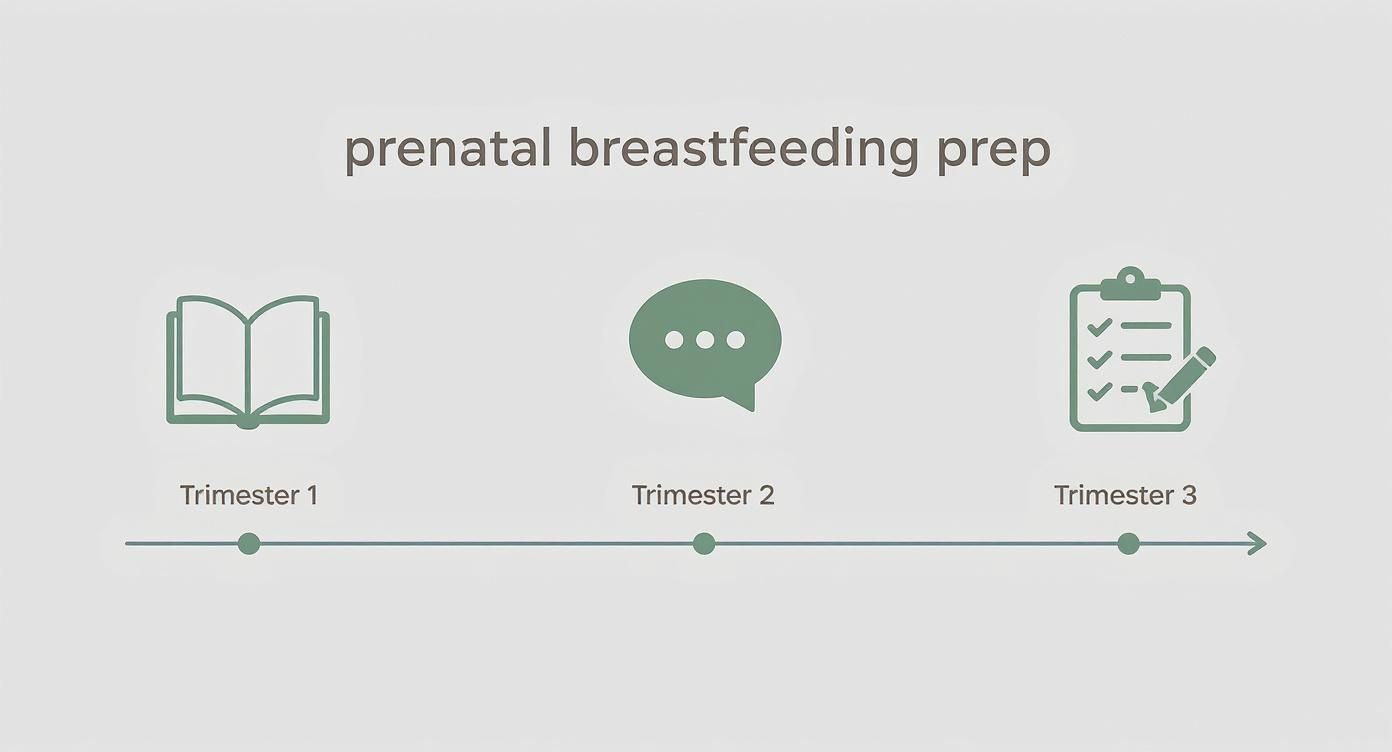
As you can see, the focus evolves—from soaking up knowledge early on to getting your home and hospital bag ready as your due date gets closer.
Cultivating a Calm Mindset
Beyond the checklists and supplies, your headspace is a huge piece of the puzzle. The newborn phase is beautiful and intense, and managing stress is absolutely essential for your well-being and your milk supply.
A confident and calm mindset is one of your most powerful breastfeeding tools. Preparation isn't just about checklists; it's about building the inner resilience to trust your body and your baby.
You can start working on this now. Explore different healthy coping mechanisms for stress, like mindfulness or simple deep-breathing exercises. These little practices can become your lifeline during a tough 3 a.m. feeding session. By learning to manage anxiety beforehand, you create a more positive, peaceful space for you and your new little one to connect.
Building Your Breastfeeding Brain Trust and Support System
Let’s be honest, getting ready for breastfeeding can feel a little like cramming for a final exam you didn’t know you had. But here's the secret: you don't have to become an expert overnight, and you absolutely shouldn't try to do it alone. The real game-changer is building your team and gathering good information before the baby arrives. It turns that feeling of "what if?" into "I've got this."

Taking this step is surprisingly powerful. One report found that an incredible 93% of parents who had a prenatal lactation consultation said it was a direct reason for their breastfeeding success. That’s a small investment of time for a massive payoff.
Finding the Right Education for You
A good prenatal breastfeeding class is so much more than a lecture. It’s your practice field. This is where you get to see what a deep, effective latch actually looks like, rather than just reading about it. Seeing it demonstrated—the asymmetrical latch, the wide-open mouth—is a world of difference from trying to decipher a diagram in a book.
You’ve got a few great options, and it’s all about finding your fit:
- Hospital-Led Classes: These are super convenient and give you the inside scoop on the hospital's specific protocols and the support you can expect during your stay.
- Private IBCLC Sessions: A one-on-one session with an International Board Certified Lactation Consultant (IBCLC) is fantastic for personalized advice. They can look at your specific anatomy and health history to give you a truly custom plan.
- Community Groups: Places like La Leche League are amazing for peer-to-peer support. You’ll hear real stories from parents who have been there, which can be incredibly reassuring.
No matter which path you choose, the goal is to walk away with a solid grasp of the basics: how milk production works, how to spot your baby's hunger cues, and what to do when you hit a common bump in the road.
Assembling Your Crew
Knowledge is crucial, but support is your lifeline. Seriously. One of the single biggest predictors of a positive breastfeeding journey is a solid support system. This crew is made up of your partner, family, friends, and the pros you line up ahead of time.
Your Partner Is Your Co-Captain Your partner's role is so much more than just being the chief water-and-snack-getter (though that is a very important job!). When they attend a class with you or read through the same info, they become an empowered advocate, not just a bystander.
"A lactation consultant is invaluable. They’re basically your breastfeeding fairy godmother, personal cheerleader, and new-parent support team all in one." - Caitlin McNeily, The Lactation Network
An informed partner can help you tweak your positioning, gently remind you of your goals when you’re exhausted and frustrated, and act as a gatekeeper for well-meaning but unhelpful advice from visitors. You can read more about the importance of family support while breastfeeding to see just how powerful a united front can be.
Finding Professional Help Before You Need It
Imagine your pipes bursting and then trying to find a good plumber at 3 a.m. That's exactly what it feels like to be frantically searching for a lactation consultant with a screaming, hungry newborn. Do the legwork now.
- Ask for Referrals: Your OB/GYN, midwife, or friends in local mom groups are the best sources for trusted IBCLCs in your area.
- Investigate Your Insurance: You might be surprised to learn that many insurance plans now cover lactation support, both before and after birth. Make a few calls to see what your policy includes.
- Book a Prenatal Consult: This is such a smart move. Meeting an IBCLC in your third trimester lets them assess any potential concerns, answer your personal questions, and get you in their system. That way, you know exactly who to text when you need help.
Getting ready for breastfeeding is less about buying all the gear and more about building a foundation of knowledge and a village of support. By putting in a little time now to learn and line up your team, you're paving the way for a much more confident and empowered start to your journey.
Prepping Your Body and Your Nursing Space
Once you have a handle on the "what" and "why" of breastfeeding, it's time to shift focus to the practical side of things—prepping your body and your home. This is all about setting yourself up for comfort and ease, creating an environment that supports you during those early, sleep-deprived days.
Let’s start with a big myth I hear all the time: that you need to "toughen up" your nipples before the baby arrives. Please don't! Old advice about rubbing them with a rough towel is completely outdated and can actually cause soreness and irritation before you even begin. A gentle, proactive approach is so much more effective.
Gentle Nipple Preparation and Care
Your body is already doing amazing things to get ready. You might notice your areolas getting darker and seeing little bumps appear—those are Montgomery glands. They secrete a natural oil that moisturizes and protects your nipples. Your job is simply to support this natural process, not work against it.
A fantastic way to do this is with a tool designed for proactive care, like Silverette® cups. These little cups are made from pure 925 sterling silver, and I’ve seen them work wonders. Silver has natural antimicrobial, anti-inflammatory, and antifungal properties that are perfect for this delicate job.
- Soothing and Healing: Silver’s natural qualities help soothe soreness or irritation without you having to slather on creams or lotions.
- Protection: The cups create a physical shield, protecting sensitive skin from rubbing against your nursing bra or clothes.
- Safe for Mom and Baby: They are completely chemical-free, so you don’t need to wash them off before nursing. That convenience is a lifesaver.
Think of Silverette® cups as a protective shield for your most sensitive skin. They don't just help after issues arise; they are a key part of a preventative strategy, creating an ideal environment for healing and comfort from day one.
If you have flat or inverted nipples, wearing Silverette cups during the last few weeks of pregnancy can be especially helpful (just be sure to get your provider's okay first). The gentle, consistent pressure can help encourage the nipple to protrude a bit, which can make it easier for your baby to get a deep, effective latch from the start.
To learn more about what to expect, check out our guide to understanding breast changes during pregnancy and how to care for yourself.
Creating Your Nursing Nook
Picture this: you’re finally settled in for a feeding session with your cluster-feeding newborn. Just as you get comfortable, you realize your phone is dead, you're desperately thirsty, and you're starving. We’ve all been there! Setting up a dedicated "nursing nook" ahead of time completely solves this problem. It’s your command center.
Find a cozy corner in your home—the nursery, the living room, your bedroom, wherever feels right—and stock it with everything you could possibly need within arm's reach.
Your Nursing Nook Checklist:
- A Comfortable Chair: A glider, rocker, or a deep armchair with good back support and armrests will be your best friend.
- Supportive Pillows: A dedicated nursing pillow is great, but also have a few extra regular pillows to prop up your arms, back, or the baby.
- Hydration and Snacks: Keep a huge water bottle (one with a straw is a game-changer for one-handed sipping!) and a stash of easy-to-eat snacks like granola bars, nuts, or dried fruit.
- Essential Supplies: Have a small basket with burp cloths, nursing pads, nipple cream (if you use it), and your Silverette cups ready to go.
- Entertainment and Tech: A long phone charger is non-negotiable. Add a book, an e-reader, or headphones for those long, quiet feeding sessions.
Beyond your physical space, preparing your body for the demands of birth and postpartum recovery is incredibly beneficial. For instance, learning how to properly strengthen your pelvic floor contributes to your overall well-being and can even make sitting for long nursing sessions more comfortable. This holistic approach—caring for both your body and your environment—truly lays the foundation for a positive start to your breastfeeding journey.
Gathering Your Breastfeeding Essentials
Stepping into the baby supply aisle can feel like entering a whole new world. There are countless gadgets, all claiming to be the one thing you can't live without. When it comes to preparing for breastfeeding, the goal is to focus on what’s genuinely helpful, not what just adds to the clutter.
Let’s cut through the noise and figure out what you really need.

The idea is to feel prepared, not buried in stuff. Having the right tools on hand from day one means you can focus on your baby instead of scrambling for a late-night store run. This prep work is more important than you might think. Studies actually show that the planning you do before birth—from gathering supplies to taking a class—has a strong link to better breastfeeding outcomes. You can read more about these important findings on breastfeeding knowledge and see just how much of a difference your efforts now can make.
Must-Haves for Day One Comfort
Think of these as your absolute non-negotiables. They’re the items that will provide the comfort and support you’ll lean on every single day.
- Supportive Nursing Bras: A few comfortable, well-fitting nursing bras are a must. Look for styles without underwire that have easy, one-handed clips for feeding. My advice? Wait until late in your third trimester to buy them to get a more accurate fit.
- Absorbent Nursing Pads: Leaks are totally normal, especially in the early days. It’s a good idea to have a mix of disposable and reusable (washable) nursing pads to keep you feeling dry and comfortable.
- A Great Nursing Pillow: This is a lifesaver for your back. A firm, supportive nursing pillow brings your baby up to breast level, which keeps you from hunching over and straining your back, neck, and shoulders.
- Silverette® Cups: Honestly, these are a game-changer for nipple care. Made from 925 sterling silver, Silverette cups act as a protective shield, preventing painful friction from your bra. Better yet, the silver has natural antimicrobial properties that help soothe and heal sore or cracked skin without needing any creams or lotions. They’re a safe and incredibly effective tool to have from the very first latch.
A well-stocked nursing station is your command center. Having these essentials within arm's reach transforms feeding time from a logistical scramble into a peaceful, bonding experience.
Nice-to-Haves That Make a Difference
Once you’ve got the basics, a few extra items can add a welcome layer of convenience and comfort. While not everyone will need these, many moms I’ve worked with find them incredibly helpful.
For more ideas, you can check out our ultimate guide to breastfeeding must-haves. Think about things like a hands-free pumping bra (a true multitasking hero!), a silicone milk collector for the opposite breast, and a big water bottle with a straw so you can stay hydrated one-handed.
Demystifying Breast Pumps
The world of breast pumps can feel overwhelming, but it really boils down to a few main types. Before you even think about buying one, make a call to your insurance company. Thanks to the Affordable Care Act, most health insurance plans are required to cover the cost of a breast pump, so you might be able to get one for free.
Here’s a quick look at your options:
| Pump Type | Best For | Key Features |
|---|---|---|
| Double Electric | Exclusive pumping or building a freezer stash | Efficient, powerful, and fast. The hospital-grade standard for milk expression. |
| Wearable/Hands-Free | Multitasking moms or pumping on the go | Discreet cups fit inside your bra, offering ultimate freedom and mobility. |
| Manual Pump | Occasional use or relieving engorgement | Lightweight, portable, and requires no electricity. Great for travel. |
Don't feel pressured to start pumping right away. For most new parents, it's best to wait 3-4 weeks to establish a strong milk supply directly with the baby. Pumping comes in handy when you’re heading back to work, if you need to be away from your baby for a bit, or if you’re working with a lactation consultant to increase your supply.
By gathering your essentials thoughtfully, you’re not just buying things—you’re building a foundation of support that will let you approach breastfeeding with confidence and calm.
Crafting Your Hospital and Postpartum Game Plan
Let’s be honest: rigid, multi-page birth plans often get tossed aside the moment things get real. But having a simple, flexible game plan for breastfeeding in the hospital? That’s empowering. It’s not about setting strict rules, but about clearly communicating your wishes so you and your care team are on the same page from the start. This lets you focus on what really matters—bonding with your baby.

That initial hospital stay is a huge piece of the puzzle. For years, global efforts to improve breastfeeding support have highlighted just how crucial a supportive maternity environment is for getting off to a good start. When mothers face early hurdles, it often traces back to a lack of preparation or inconsistent in-hospital support. Thinking through your hospital plan is one of the most important first steps you can take.
Your Hospital Breastfeeding Checklist
Think of this less as a formal document and more as a conversation starter for your nurses and doctors. You can jot these down or just keep them in mind to discuss when you arrive.
- Immediate Skin-to-Skin: Ask for uninterrupted skin-to-skin contact for at least the first hour after birth (or as soon as it's medically safe). This simple act helps regulate your baby's temperature and heart rate and kicks your own breastfeeding hormones into high gear.
- Nurse During the "Golden Hour": That first hour of life is often when your baby is most alert and instinctively ready to feed. Let your team know you want to try the first latch during this special window.
- Rooming-In: Request that your baby stays in your room with you 24/7. This is the best way to learn their early hunger cues—like rooting or bringing their hands to their mouth—before they escalate to full-blown crying. It makes for much calmer feedings.
- Lactation Support: Ask if an IBCLC (International Board Certified Lactation Consultant) is on staff and request a visit within the first 24 hours. They are the experts and can help you nail down positioning and latch from the very beginning, preventing many common problems before they start.
- Preferences on Supplements: Make it clear that you prefer no pacifiers, formula, or sugar water unless it’s medically necessary and you’ve discussed it first. This helps ensure your baby is focused on learning to breastfeed.
Surviving and Thriving in the First Weeks Home
Once you’ve settled in at home, your world shrinks to a rhythm of rest, recovery, and round-the-clock feedings. The intensity can be surprising, but knowing what’s coming makes it all feel more manageable. Your mission is simple: feed the baby, rest when you can, and protect your milk supply.
"The first two weeks postpartum are a sacred window. Protect this time fiercely. Your only jobs are to snuggle your baby, learn their cues, and nourish both of you. Everything else can wait."
During this period, remember that breastfeeding is all about supply and demand. The more frequently and effectively your baby nurses, the more milk your body will produce.
What to Realistically Expect Postpartum
- Cluster Feeding Marathons: Get ready for times when your baby wants to nurse almost constantly, sometimes for hours on end. This is totally normal behavior. It’s how they fuel growth spurts and tell your body to ramp up milk production.
- Engorgement: Around day three or four, your mature milk will "come in." For many, this causes breasts to feel incredibly full, firm, and tender. The best remedy is frequent nursing. For extra relief, you can use a warm compress before feeding to help with letdown and a cold compress after to reduce swelling.
- Nipple Tenderness: It's really common to feel some tenderness as your body adjusts during that first week. This is where a little preparation pays off. To manage this, wear your Silverette cups between every feeding. The silverettes protect your delicate skin from the friction of your bra and create an environment that promotes natural healing. Having these silverettes ready from day one is a key part of preparing for breastfeeding before baby arrives and can help you move through this adjustment period much more comfortably. You can learn more about how Silverette can support your breastfeeding journey.
Common Questions on Breastfeeding Preparation
https://www.youtube.com/embed/bNOlJBNskrA
As your due date gets closer, it's completely normal for a million little questions to start swirling in your head. And while every single breastfeeding experience is different, you'd be surprised how many of us share the exact same worries.
Let's clear the air and tackle some of the most common questions I hear from expectant parents. Getting these answers now can help you walk into this new chapter feeling calm and ready.
When Is the Best Time to Start Preparing for Breastfeeding?
The third trimester is really the sweet spot. Any earlier, and the information can feel a bit abstract. But once you’re in those final months, everything becomes much more real.
A great time to take a class or meet with a lactation consultant is around the 30-34 week mark. The information will be fresh in your mind right when you need it most, and you’ll have time to ask questions and gather any last-minute supplies without feeling frantic.
Of course, you can start your basic research or buy things like nursing bras or Silverette® cups whenever you feel ready. But for that practical, hands-on learning, waiting until a bit closer to your due date is usually most effective.
Do I Really Need a Class if I've Read Books?
I’m a huge fan of books and online resources for building a solid foundation of knowledge. But a live class, whether in-person or virtual, offers something you just can't get from a book. It’s the difference between reading a recipe and actually having a chef show you how to chop the vegetables.
A class led by an International Board Certified Lactation Consultant (IBCLC) gives you:
- Live Demonstrations: Seeing an expert use a doll to demonstrate a deep, effective latch is so much clearer than trying to decipher a diagram. It just clicks.
- Interactive Q&A: This is your chance to ask your specific questions and hear what other parents are asking. It’s incredibly validating to know you’re not the only one wondering about something.
- A Sense of Community: Simply being with other people who are on the exact same journey is powerful. It reminds you that you aren't in this alone.
So while reading is great, the dynamic and visual nature of a class can give your confidence a serious boost.
How Can My Partner Best Support My Breastfeeding Goals?
Partner support is a game-changer. Seriously, it's one of the biggest predictors of breastfeeding success. When your partner is an active, clued-in participant, it transforms the entire postpartum experience from a solo mission into a team effort.
The single most helpful thing a partner can do is become an educated advocate. Their job isn’t just to bring you water (though that’s important!). It’s to be a reassuring presence who understands the basics and can help you troubleshoot when you’re exhausted.
Here are a few powerful ways they can step up:
- Take the Class With You: When you both hear the same information, you're on the same team. You’ll share the same vocabulary, goals, and understanding of when to call for help.
- Be the "Nursing Station Manager": They can take ownership of keeping your favorite spot stocked with snacks, a full water bottle, burp cloths, your phone charger, and anything else you need to feel comfortable.
- Act as Your Cheerleader and Gatekeeper: This is maybe the most important role. They can offer a word of encouragement when you’re feeling defeated, gently fend off unhelpful advice from well-meaning visitors, and handle diaper changes so you can focus on feeding.
Can I Still Breastfeed With Flat or Inverted Nipples?
Yes, absolutely! This is such a common worry, but please know that countless parents with flat or inverted nipples go on to breastfeed successfully. Remember, a baby latches onto the areola, not just the very end of the nipple. A deep latch is key.
That said, a little extra preparation can make things go more smoothly. I always recommend meeting with an IBCLC before you deliver. They can assess your specific situation and give you personalized tips and techniques. If you're concerned about this, our guide on understanding and addressing latching difficulties in breastfeeding offers more detailed advice.
This is also a situation where Silverette® cups can be a great addition to your toolkit. With your doctor or midwife’s okay, wearing silverettes in the final weeks of pregnancy can apply a gentle, steady pressure that helps encourage the nipple to evert, which can make those first few latches a little easier for your baby. Plus, the natural properties of silverettes help soothe and protect your skin before your nursing journey even officially begins.
At MoogCo, we believe that feeling prepared is the foundation for a confident and comfortable nursing experience. Our Original Silver Nursing Cups are a simple, effective tool to have in your prenatal kit, offering soothing relief and protection right from the start.
Discover how MoogCo Silverette cups can support your breastfeeding journey from the very start.